Causes, Symptoms, and Solutions of Itchy Teeth

Itchy teeth might sound unusual, but they are a common concern. Around 50% of dental patients sometimes report discomfort like itchiness in their teeth or gums. This sensation is often overlooked, yet it can indicate underlying dental issues that require attention. If you’ve ever wondered why your teeth itch or how to stop it, this article will answer. What Are Itchy Teeth? Itchy teeth occur when you experience an unusual tingling or scratching sensation on your teeth or gums. This feeling might not be painful, but it can be annoying and persistent. Knowing what causes this sensation is the first step in addressing it effectively. Why Itchy Teeth Happen The sensation of itchy teeth can be linked to several factors, including allergies, gum disease, or even a reaction to certain dental products. According to dental health studies, around 60% of people with itchy teeth might suffer from gum disease or allergic reactions. These statistics highlight the importance of addressing itchiness in teeth early before it leads to more severe issues. Common Causes of Itchy Teeth Recognizing the underlying cause of your itchy teeth is crucial for proper treatment. Here are the most common causes: 1. Gum Disease Gum disease is a prevalent condition affecting nearly 47.2% of adults over 30. It often begins with plaque buildup, leading to inflammation of the gums. If left untreated, this inflammation can cause your gums to itch as the body reacts to the bacteria present. How to Prevent Gum Disease 2. Allergic Reactions Allergies can cause your immune system to overreact, leading to itchy gums and teeth. Common allergens include certain foods, dental products, and seasonal pollen. It may be an allergic reaction if your teeth itch after using a new toothpaste or eating specific foods. 3. Dry Mouth (Xerostomia) Dry mouth is another common cause of itchy teeth. Approximately 10% of people suffer from xerostomia, a condition where your mouth doesn’t produce enough saliva. Saliva helps to cleanse your mouth and prevent bacteria buildup. Without enough saliva, your mouth can become dry, leading to an itchiness sensation in your gums and teeth. 4. Braces or Retainers Wearing braces or retainers can sometimes cause itchy teeth, especially if improperly cleaned. Food particles can get trapped, leading to bacterial growth and irritation. Regular cleaning of these dental devices is essential to prevent this discomfort. Invisalign vs Braces: Comparison for Your Orthodontic Journey 5. Oral Thrush Oral thrush is a fungal infection that affects the mouth. It’s more common in people with weakened immune systems, affecting nearly 5-7% of infants and older adults. Oral thrush can cause white patches on the gums, a burning sensation, and sometimes itchy teeth. Symptoms Accompanying Itchy Teeth Other symptoms often accompany itchiness in teeth. These symptoms can help your dentist diagnose the cause of your discomfort: Red, Swollen Gums: Inflammation of the gums is a common sign of gum disease or an allergic reaction. Bad Breath: Persistent bad breath can indicate bacterial buildup, often linked to dry mouth or gum disease. Sensitivity to Hot or Cold: Teeth sensitivity is sometimes related to itchy teeth, particularly if the itchiness is caused by gum recession or tooth enamel erosion. Bleeding Gums: Bleeding during brushing or flossing is another sign of gum disease, which could be contributing to itchiness. Recognizing these symptoms early can help prevent more serious dental issues. How to Address Itchy Teeth: Practical Solutions If you’re experiencing itchy teeth, several practical steps can help alleviate the discomfort. Addressing the root cause is key to long-term relief. 1. Improve Oral Hygiene to Prevent from Itchy Teeth Good oral hygiene is essential for preventing and treating itchiness. Brushing twice daily with fluoride toothpaste and flossing daily can help remove plaque and prevent gum disease. A dental survey found that people who follow a strict oral hygiene routine are 30% less likely to experience gum-related issues. 2. Visit Your Dentist Regularly Regular dental check-ups are crucial for maintaining healthy teeth and gums. Dentists can identify early signs of gum disease or other conditions that might cause itchiness. It’s recommended to visit your dentist at least twice a year. How to Find a Good Dentist Near You 3. Use Hypoallergenic Dental Products If you suspect your itchy teeth are due to an allergic reaction, switching to hypoallergenic dental products might help. Look for toothpaste and mouthwash that is free from common allergens like sodium lauryl sulfate or artificial flavors. 4. Stay Hydrated for Itchy Teeth Drinking plenty of water throughout the day can help prevent dry mouth, a common cause of itchiness. Water helps to stimulate saliva production, which is essential for keeping your mouth clean and free from bacteria. 5. Treat Underlying Conditions If your itchy teeth are due to a condition like oral thrush or dry mouth, treating these conditions can alleviate the itchiness. Over-the-counter antifungal treatments can help with oral thrush while moisturizing mouth sprays can relieve dry mouth symptoms. Preventing Itchy Teeth: Long-Term Care Preventing itchy teeth involves taking proactive steps to maintain your oral health. Here are some tips to keep your teeth and gums healthy: 1. Maintain a Balanced Diet A balanced diet rich in vitamins and minerals is essential for strong teeth and healthy gums. Eating foods high in calcium, like dairy products, can help strengthen your teeth, while fruits and vegetables can provide the vitamins your gums need to stay healthy. 2. Avoid Tobacco Products Tobacco use is a leading cause of gum disease, which can lead to itchy teeth. Quitting smoking or avoiding tobacco products can significantly reduce your risk of developing gum-related issues. 3. Wear a Mouthguard If you grind your teeth at night, wearing a mouthguard can prevent damage to your teeth and gums. Teeth grinding, known as bruxism, can lead to tooth wear and gum recession, which can cause itchiness. 4. Regular Dental Cleanings Professional dental cleanings remove plaque and tartar that regular brushing can’t reach. Regular cleanings, usually every six months, can help prevent gum
Periodontal vs. Gingivitis: Understanding the Differences

Regarding dental health, two common terms often arise gingivitis and periodontal disease. Both conditions relate to the health of your gums, but they are not the same. According to the Centers for Disease Control and Prevention (CDC), nearly 47% of adults over 30 suffer from some form of periodontal disease. Knowing the differences between these two conditions is essential for proper treatment and prevention. This article will explain the differences, causes, symptoms, and treatments of gingivitis vs periodontal disease. What Is Gingivitis? Gingivitis is the mildest form of gum disease. It’s an early stage where the gums become inflamed due to plaque buildup on the teeth. Gingivitis is reversible with proper care, making it essential to catch and treat it early. The primary cause of gingivitis is poor oral hygiene. When you don’t brush or floss regularly, plaque, a sticky film of bacteria, forms on your teeth. Over time, this plaque irritates your gums, leading to inflammation and bleeding during brushing or flossing. The good news is that gingivitis can be controlled with regular brushing, flossing, and professional cleanings. What Is Periodontal Disease? If gingivitis is left untreated, it can progress to a more severe condition known as periodontal disease. The CDC reports that periodontal disease affects nearly 70% of adults aged 65 and older. This condition is much more serious because it involves the gums and the bones supporting your teeth. Once periodontal disease advances, it can lead to tooth loss if not treated promptly. Periodontal disease occurs when plaque spreads below the gum line. The bacteria in plaque produce toxins that irritate the gums and cause inflammation. This inflammation causes the gums to pull away from the teeth, forming pockets. These pockets become infected, and as the disease progresses, the bones, gums, and connective tissue that support the teeth are destroyed. Without treatment, the teeth may eventually become loose and fall out. Symptoms: How to Identify Gingivitis vs Periodontal Disease It’s important to recognize the symptoms of gingivitis and periodontal disease to seek timely treatment. Here’s how you can differentiate between these two: Gingivitis Symptoms: Red, swollen gums that bleed easily during brushing or flossing. The gums may feel tender, but there’s usually no pain at this stage. You might also notice bad breath (halitosis). Periodontal Disease Symptoms: Symptoms are more severe and may include receding gums, deep pockets between teeth and gums, loose or shifting teeth, pus between the teeth and gums, and persistent bad breath. As the disease progresses, you may experience pain while chewing, and your teeth may become loose or fall out. Causes of Periodontal vs Gingivitis Disease Understanding the causes of gingivitis and periodontal disease can help you prevent these conditions. According to the World Health Organization (WHO), gum diseases are the 11th most prevalent disease globally. The causes can vary, but some common factors include: Poor Oral Hygiene: The most common cause of gingivitis is poor oral hygiene. Not brushing and flossing regularly allows plaque to build up, leading to inflammation of the gums. Smoking: Tobacco use is a significant risk factor for periodontal disease. Smokers are seven times more likely to develop gum disease than non-smokers. Hormonal Changes: Women may experience gum inflammation during pregnancy, menstruation, or menopause due to hormonal fluctuations. Medical Conditions: Certain diseases, such as diabetes, can increase the risk of developing gum disease. People with diabetes are more likely to develop infections, including periodontal disease. Medications: Some medications can reduce saliva flow, leading to a dry mouth and increasing gum disease risk. Learn more about Gingivitis: Does Hydrogen Peroxide Cure Gingivitis? Exploring Its Role in Oral Health Treatment Options: What Can Be Done for Periodontal vs Gingivitis? When treating gingivitis and periodontal disease, the earlier you start, the better. For gingivitis, the treatment is straightforward. Good oral hygiene is often enough to reverse the condition. Regular brushing, flossing, and professional cleanings can remove plaque and prevent gingivitis from worsening. Your dentist may also recommend an antibacterial mouthwash to reduce plaque and bacteria. For periodontal disease, the treatment depends on the severity of the condition. In the early stages, scaling and root planning can be effective. This deep cleaning removes plaque and tartar below the gum line and smooths the tooth roots to help the gums reattach. Surgical treatments like flap surgery, bone grafts, or tissue regeneration may be necessary if the disease has advanced. What Happens If Left Untreated Periodontal vs Gingivitis? Ignoring gingivitis or periodontal disease can have serious long-term consequences. The CDC states that gum disease is the leading cause of tooth loss in adults. Without proper treatment, gingivitis can progress to periodontal disease, leading to irreversible damage to your gums and the supporting structures of your teeth. Untreated Gingivitis: If left untreated, gingivitis can lead to periodontitis, which can cause the gums to recede and form pockets. These pockets can infect and destroy the tissue and bone supporting your teeth. This process can result in tooth loss and may even affect your overall health, as periodontal disease has been linked to conditions like heart disease, diabetes, and respiratory issues. Untreated Periodontal Disease: The consequences are even more severe. As the disease progresses, the pockets deepen, and more gum tissue and bone are destroyed. Teeth may become loose and eventually fall out or need to be removed. Advanced periodontal disease can also lead to systemic issues, as the bacteria from the infection can enter the bloodstream and affect other parts of the body. Conclusion: Taking Control of Your Gum Health Gum health is vital to your overall well-being. According to the ADA, untreated gum disease can lead to serious health problems, including heart disease and stroke. Understanding the difference between gingivitis and periodontal disease is the first step in taking control of your gum health. You can prevent gum disease and maintain a healthy smile by practising good oral hygiene, quitting smoking, and visiting your dentist regularly. Remember, early detection is key to preventing the progression
Understanding the Dangers of a Tooth Infection
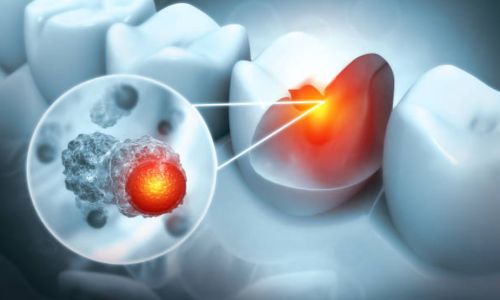
Tooth infections, if left untreated, can pose serious health risks, potentially leading to life-threatening complications. This article will explore tooth infection kills, the associated risks, and the importance of timely intervention. What is a Tooth Infection? A tooth infection, also known as a dental abscess, occurs when bacteria invade the tooth’s pulp, forming pus. This can result from untreated cavities, cracked teeth, or gum disease. The infection can cause significant pain, swelling, and other symptoms, indicating the need for immediate dental care. Symptoms of a Tooth Infection Recognizing the symptoms of a tooth infection is crucial for seeking timely treatment. Common symptoms include: Severe Toothache A persistent, throbbing toothache is one of the most common and noticeable symptoms of a tooth infection. This pain can be quite severe and continuous, making it difficult to ignore. The pain is often described as sharp or shooting and may intensify when you lie down. The toothache may also radiate to the jawbone, neck, or ear on the same side as the infected tooth. This discomfort is typically a result of the infection spreading to the nerves in the tooth’s root, causing inflammation and intense pain. Swelling Swelling is another prominent symptom of a tooth infection. The gums around the affected tooth may become swollen, red, and tender. This swelling can extend to the face or jaw, leading to visible puffiness and discomfort. In some cases, the swelling can be so significant that it causes difficulty in opening the mouth, eating, or speaking. This symptom indicates the infection has spread beyond the tooth and affects the surrounding tissues. Fever A fever may develop as your body’s immune system fights the infection. An elevated body temperature indicates that your body responds to the bacterial invasion. Along with fever, you might experience general malaise, fatigue, and feeling unwell. A fever suggests that the infection is more severe and that medical attention is needed promptly. Bad Breath: Tooth Infection Kills Bad breath, also known as halitosis, is a common symptom of a tooth infection. The pus and decaying tissues within the infected tooth can lead to a foul smell or taste in your mouth. This unpleasant odour persists despite regular brushing and mouthwash use. It is often a clear indication of an underlying infection that needs to be addressed. Sensitivity Increased sensitivity to hot or cold temperatures can indicate a tooth infection. You might feel sharp pain when consuming hot drinks, cold foods, or even when breathing in cold air. This sensitivity occurs because the infection irritates the nerve endings within the tooth, making it more reactive to temperature changes. Swollen Lymph Nodes The lymph nodes under your jaw or neck may become swollen and tender when a tooth infection occurs. These nodes are part of your body’s immune system and become enlarged as they work to fight off the infection. Swollen lymph nodes can be painful to the touch and a sign that the disease spreads beyond the tooth. Complications of Untreated Tooth Infection Kills If a tooth infection is left untreated, it can spread to other parts of the body, leading to severe and potentially fatal complications: Abscess Spread If a tooth infection is left untreated, the disease can spread from the tooth to the surrounding tissues, forming a larger abscess. This can lead to increased pain, swelling, and more severe infection. An abscess is a pocket of pus that can cause significant discomfort and may need to be drained by a dentist. Bone Infection (Osteomyelitis) Bacteria from a tooth infection can spread to the bones supporting the teeth, causing a condition known as osteomyelitis. This infection of the bone can cause severe pain, swelling, and fever. Osteomyelitis requires prompt medical treatment, often including antibiotics and sometimes surgery, to remove the infected bone tissue. Cellulitis A tooth infection can spread to the skin and soft tissues, leading to cellulitis. This serious bacterial infection causes redness, swelling, and pain in the affected area. Cellulitis can spread rapidly and become life-threatening if it enters the bloodstream. Immediate medical treatment is essential to prevent severe complications. Sepsis If a tooth infection spreads to the bloodstream, it can lead to severe and potentially fatal sepsis. Sepsis is the body’s extreme response to an infection and can cause widespread inflammation, leading to organ failure and septic shock. Symptoms of sepsis include high fever, rapid heart rate, difficulty breathing, and confusion. Sepsis is a medical emergency that requires immediate treatment in a hospital. Sepsis is a leading cause of death in the United States, with a mortality rate of over 215,000 deaths per year. Source. Ludwig’s Angina Ludwig’s angina is a type of severe cellulitis that occurs on the floor of the mouth. It causes swelling, difficulty breathing, and difficulty swallowing and can rapidly become life-threatening. This condition requires emergency medical treatment, including antibiotics and sometimes surgery, to secure the airway and treat the infection. How Long Until a Tooth Infection Kills? The timeline for a tooth infection to become life-threatening can vary widely depending on several factors, including the individual’s overall health, the severity of the disease, and how quickly it spreads. In some cases, a tooth infection can lead to severe complications very rapidly, while in other cases, it might take weeks or even months to progress to a life-threatening stage. Immediate Danger: Tooth Infection Kills Sometimes, a tooth infection can quickly escalate, leading to severe symptoms such as difficulty breathing or swallowing. These symptoms are medical emergencies and require immediate attention. Rapid progression can be especially dangerous for individuals with weakened immune systems or other underlying health conditions. Gradual Progression The infection may cause persistent symptoms for many people that gradually worsen over time. The disease can spread to surrounding tissues and other body parts without treatment, leading to serious health issues. Regular monitoring and early intervention are key to preventing the disease from reaching a critical stage. Importance of Timely Treatment To prevent complications, seeking prompt dental care at the first sign of a
How to Have Beautiful Teeth

Beautiful teeth not only enhance your smile but also boost your confidence. Achieving and maintaining a radiant smile involves a combination of good oral hygiene, regular dental visits, and a healthy lifestyle. Understanding how to have beautiful teeth can help you enjoy a stunning smile for years. “A gap-free smile is considered more attractive by 90% of people surveyed.” Sources Importance of Beautiful Teeth Beautiful teeth play a significant role in your overall appearance and self-esteem. A bright, white smile can make a positive impression and enhance your confidence in social and professional settings. Healthy teeth also contribute to better oral health, reducing the risk of cavities, gum disease, and other dental issues. Prioritizing your dental care can lead to a more attractive and healthier smile. Practicing Good Oral Hygiene Good oral hygiene is the foundation of beautiful teeth. Regular brushing, flossing, and rinsing help remove plaque and prevent cavities. Proper oral hygiene also keeps your gums healthy, reducing the risk of gum disease. Incorporating these habits into your daily routine is essential for maintaining a bright and healthy smile. Brushing Brushing your teeth twice daily is crucial for removing food particles and plaque. Use a fluoride toothpaste and a soft-bristled toothbrush. Brush for at least two minutes, making sure to clean all surfaces of your teeth. Pay special attention to the gum line, as plaque can accumulate and cause gum disease. Flossing Flossing helps remove plaque and food particles between your teeth, which your toothbrush can’t reach. Floss at least once daily, using a gentle sawing motion to avoid injuring your gums. Proper flossing can prevent cavities and gum disease, creating a healthier and more beautiful smile. Rinsing Rinsing with an antiseptic mouthwash can help kill bacteria and freshen your breath. Mouthwash can also reduce plaque and prevent gum disease. Rinse your mouth with mouthwash after brushing and flossing to enhance your oral hygiene routine and keep your teeth and gums healthy. Regular Dental Visits Regular dental visits are essential for maintaining beautiful teeth. Your dentist can detect and address dental issues early, preventing them from becoming more severe. Professional cleanings remove plaque and tartar buildup, keeping your teeth clean and healthy. Regular check-ups also allow one to discuss concerns and receive personalized advice on maintaining your smile. Professional Cleanings Professional cleanings remove plaque and tartar that brushing and flossing can’t reach. Your dentist or hygienist will use specialized tools to clean your teeth thoroughly, including below the gum line. Regular cleanings prevent cavities, gum disease, and other dental issues, contributing to a healthier and more attractive smile. Dental Check-Ups Regular dental check-ups allow your dentist to monitor your oral health and detect any issues early. During a check-up, your dentist will examine your mouth, gums and mouth for signs of cavities, gum disease, and other problems. Early detection and treatment can prevent more severe issues and help maintain your beautiful smile. Healthy Diet and Lifestyle A healthy diet and lifestyle play a crucial role in maintaining beautiful teeth. Certain foods and habits can affect oral health, so making mindful choices is essential. Avoiding sugary foods and drinks, staying hydrated, and quitting smoking can significantly impact the health and appearance of your dentures. Avoid Sugary Foods and Drinks Sugary foods and drinks can contribute to tooth decay and cavities. Bacteria in your mouth feed on sugar, producing acids that erode your tooth enamel. Limit your consumption of sugary snacks, candies, and sodas. Opt for healthier alternatives like fruits, vegetables, and water. Stay Hydrated Staying hydrated is essential for your overall health and oral health. Drinking plenty of water helps rinse away food particles and bacteria, reducing the risk of cavities and gum disease. Water also stimulates saliva production, which helps neutralize acids and protect. Quit Smoking Smoking can significantly negatively impact your oral health and the appearance of your teeth. Tobacco use can cause yellowing, staining, and bad breath. It also increases the risk of gum disease and oral cancer. Quitting smoking can improve health and contribute to a more beautiful smile. Teeth Whitening Teeth whitening is a popular cosmetic procedure that can enhance the appearance of your smile. There are various methods available, including professional treatments and at-home options. Understanding the benefits and risks of teeth whitening can help you make an informed decision. Professional Teeth Whitening Your dentist performs professional teeth whitening and offers the most effective results. The procedure typically involves applying a bleaching agent and using a special light to enhance the whitening process. Professional whitening can lighten your teeth in just one visit, providing a brighter and more radiant smile. At-Home Teeth Whitening At-home teeth whitening kits are available over the counter and can be a convenient option for enhancing your smile. These kits usually include whitening strips, gels, or trays you apply to your teeth. While at-home treatments may not be as effective as professional whitening, they can still provide noticeable results. It’s essential to follow the instructions carefully to avoid potential side effects. Correcting Dental Issues Correcting dental issues is essential for achieving and maintaining beautiful teeth. Misaligned, chipped, or missing can affect the appearance of your smile and your oral health. Various treatments, including orthodontics, veneers, and dental implants, are available to address these issues. Orthodontics Orthodontic treatments, such as braces and clear aligners, can correct misaligned teeth and improve your bite. Straightening your teeth enhances your smile and makes it easier to clean your teeth and maintain good oral hygiene. Orthodontic treatments can significantly improve the appearance and health. Veneers Veneers are thin shells of porcelain or composite resin bonded to the front of your incisors. They can correct cosmetic issues, including discolouration, chips, and gaps. Veneers provide a natural-looking solution for enhancing the appearance of your smile. Dental Implants Dental implants are a permanent solution for replacing missing tooth. They consist of a titanium post that is surgically placed into your jawbone and a crown that is attached to the post. Dental implants look and function like natural
Tooth Cupping Treatment: Causes, Procedures, and Prevention

Tooth cupping, a dental condition where small, cup-like depressions form on the chewing surfaces of teeth, can cause discomfort and affect oral health. Understanding the causes, treatment options, and preventive measures is essential for maintaining a healthy smile. This article will explore tooth cupping treatment in detail, offering valuable insights for anyone seeking to address this issue. Nearly 1 in 4 older adults over 75 are edentulous (toothless). The prevalence of toothlessness is higher in low-income groups (13%) and among those who did not graduate high school (15%). Source. What is Tooth Cupping? Tooth cupping refers to the formation of small indentations or cups on the surface of the teeth, particularly the molars and premolars. These indentations can vary in size and depth and become more pronounced over time. Tooth cupping can increase tooth sensitivity, discomfort while chewing, and even structural damage if left untreated. Causes of Tooth Cupping Acid Erosion One of the primary causes of tooth cupping is acid erosion. Acidic foods and beverages, such as citrus fruits, soda, and certain juices, can wear away the enamel, the protective outer layer of the teeth. When enamel erodes, it exposes the underlying dentin, which is softer and more susceptible to wear and tear. Over time, this erosion can lead to cupped areas on the tooth surface. Bruxism Bruxism, or teeth grinding, is another common cause of tooth cupping. People who grind their teeth, especially at night, put excessive pressure on their teeth, leading to wear and tear. This constant grinding can cause the enamel to wear down, resulting in the characteristic cupped appearance of the teeth. Bruxism can be related to stress, anxiety, or sleep disorders. Poor Oral Hygiene Poor oral hygiene practices can also contribute to tooth cupping. Inadequate brushing and flossing allow plaque and bacteria to accumulate on the teeth. Over time, this buildup can lead to the demineralization of the enamel, making it more prone to erosion and cupping. Maintaining good oral hygiene is crucial to preventing this condition. Dietary Habits Dietary habits play a significant role in tooth cupping. Consuming a diet high in sugary and acidic foods can accelerate enamel erosion. Frequent snacking on such foods increases the exposure of teeth to harmful acids, contributing to the development of cupped areas. It’s important to be mindful of your diet to protect your teeth from cupping. Symptoms of Tooth Cupping Increased Sensitivity One of the most common symptoms of tooth cupping is increased sensitivity. As the enamel wears away and the dentin becomes exposed, the teeth become more sensitive to hot, cold, sweet, and acidic foods and beverages. This sensitivity can cause discomfort and make eating and drinking unpleasant. Visible Indentations Visible indentations or cups on the chewing surfaces of the teeth characterize tooth cupping. These indentations can vary in size and depth and become more noticeable as the condition progresses. Regular dental check-ups can help identify these indentations early and prevent further damage. Discomfort While Chewing People with tooth cupping may experience discomfort or pain while chewing. The exposed dentin is more susceptible to pressure and can cause discomfort when chewing certain foods. This discomfort can affect eating habits and overall oral health. Increased Risk of Cavities Tooth cupping can increase the risk of cavities. The indentations created by cupping can trap food particles and bacteria, making it harder to keep the teeth clean. If not properly addressed, this trapped debris can lead to tooth decay and cavities. Regular dental cleanings and good oral hygiene can help prevent cavities. Diagnosis of Tooth Cupping Dental Examination A dental examination is the first step in diagnosing tooth cupping. During the examination, the dentist will visually inspect the teeth for any signs of cupping, such as indentations or wear on the chewing surfaces. The dentist may also use dental instruments to check for sensitivity or discomfort in the affected areas. Dental X-rays Dental X-rays can provide valuable information about the extent of tooth cupping. X-rays can reveal any underlying damage or structural issues that may not be visible during a visual examination. The dentist can use this information to develop an appropriate treatment plan and monitor the condition’s progress. Assessing Oral Habits Assessing oral habits is another important aspect of diagnosing tooth cupping. The dentist will ask about your dietary habits, oral hygiene practices, and teeth grinding or clenching history. This information can help identify potential causes of tooth cupping and guide the treatment plan. Treatment Options for Tooth Cupping Fluoride Treatment Fluoride treatment is one of the most effective ways to strengthen the enamel and protect against tooth cupping. It helps remineralize the enamel, making it more resistant to acid erosion and wear. Dentists can apply fluoride treatments during regular check-ups or use fluoride toothpaste and mouthwash at home for added protection. Dental Bonding Dental bonding is a cosmetic procedure that can address minor cases of tooth cupping. During the procedure, the dentist applies a tooth-coloured resin to the affected areas, filling in the indentations and restoring the tooth’s surface. Dental bonding can improve the appearance of the teeth and reduce sensitivity. Dental Crowns in Tooth Cupping Treatment For more severe cases of tooth cupping, dental crowns may be necessary. Dental crowns are custom-made caps that cover the entire tooth, providing protection and restoring its shape and function. Crowns can prevent further damage and improve the overall strength and appearance of the teeth. Custom Mouthguards If bruxism contributes to tooth cupping, custom mouthguards can help protect the teeth. Mouthguards are worn at night to prevent teeth grinding and clenching, reducing the pressure on the teeth and minimizing wear. Custom mouthguards are designed to fit your teeth perfectly, providing optimal protection. Dietary Changes Making dietary changes can also help treat and prevent tooth cupping. Reducing the intake of sugary and acidic foods and beverages can protect the enamel from erosion. A balanced diet of calcium and other essential nutrients supports healthy teeth and gums. Preventive Measures for Tooth Cupping Treatment Maintain Good Oral Hygiene
Do Braces Go on Molars?

When most people think of braces, they often envision brackets and wires on the front teeth. However, the role of molars in orthodontic treatment is crucial. This article aims to answer the question: do braces go on molars? Understanding the placement and function of braces on molars can help you better appreciate the intricacies of orthodontic treatment. Understanding the Role of Molars in Orthodontics Molars are the large, flat teeth at the back of your mouth. They play a significant role in chewing and grinding food. Their position and function are critical in maintaining proper teeth and jaw alignment. Considering the molars’ role in the overall dental structure is essential. Proper alignment of molars ensures a stable and functional bite, which is vital for oral health. Why Do Braces Go on Molars? Orthodontists often place braces on molars for several reasons. Molars serve as anchor points to move other teeth into their correct positions. By attaching braces to molars, orthodontists can apply the necessary force to shift teeth effectively. Moreover, aligning molars is important for achieving a balanced bite. Misaligned molars can lead to uneven wear on teeth, jaw pain, and other dental issues. Types of Braces Metal Braces: These are the traditional braces made of high-grade stainless steel. They are the most common type and are very strong, making them suitable for molars, which require a lot of force to move. Ceramic Braces: These are similar to metal braces but are made of clear or tooth-colored material. They are less noticeable but can be more fragile than metal braces. Lingual Braces: These braces are placed on the back side of the teeth, making them invisible from the front. They can be customized to fit each tooth but might be more uncomfortable initially. Self-Ligating Braces: These braces use a special clip instead of elastics to hold the wire. They can be metal or ceramic and often require fewer adjustments, making the treatment faster. Four million Americans, mainly teens (80%), wear braces. Meanwhile, nearly 25 to 50% of all children will also be braces-wearers. Source. How Braces on Molars Affect Treatment Braces on molars play a significant role in the overall orthodontic treatment process. They help distribute the pressure the braces apply across all teeth. This distribution is essential for moving teeth into their correct positions. Achieving the desired results without bracing on the molars would be challenging. Therefore, when considering “do braces go on molars,” it’s important to understand their impact on the treatment’s effectiveness and efficiency. Do Braces Go on Molars for All Patients? While braces on molars are common, they may not be necessary for every patient. The decision to place braces on molars depends on various factors, including the patient’s age, the severity of the misalignment, and the specific treatment plan. For example, younger patients with developing jaws might not require braces on molars initially. However, as treatment progresses, the orthodontist may decide to include molars. Thus, the answer to “Do braces go on molars?” can vary, but they are often essential for comprehensive treatment. The Process of Placing Braces on Molars Consultation: The orthodontist examines your teeth and takes X-rays and impressions to plan the treatment. Cleaning: Before placing the braces, the teeth are thoroughly cleaned to ensure no food particles or plaque are left. Bonding: The orthodontist applies a special adhesive to the molars and attaches the brackets. These brackets are the small squares that will hold the wires. Placing the Archwire: The archwire is threaded through the brackets. This wire applies pressure to the teeth to move them into the desired position. Adding Ligatures: Tiny rubber bands or clips are placed to hold the archwire in the brackets. Adjustments: The orthodontist will adjust the braces over time by tightening the wires to gradually move the teeth into place. Challenges of Braces Accessibility: Molars are at the back of the mouth, making it harder for the orthodontist to place and adjust the braces. It can also be difficult for you to clean around them properly. Discomfort: Braces on molars can cause more discomfort or soreness than other teeth because molars are larger and require more force to move. This can lead to pressure and pain, especially after adjustments. Risk of Breakage: Molars do a lot of heavy chewing, which puts extra stress on the braces. This increases the risk of brackets or wires breaking or coming loose, possibly requiring additional visits to the orthodontist for repairs. Care and Maintenance of Braces on Molars Proper care and maintenance of braces on molars are crucial for successful orthodontic treatment. Patients should brush and floss regularly, paying special attention to the molars. Using interdental brushes or water flossers can help clean around the brackets and wires. Additionally, patients should avoid hard and sticky foods that can damage the braces. Regular dental check-ups and adjustments are essential to ensure the treatment progresses as planned. Overview of Do Braces Go on Molars Molars play a critical role in orthodontic treatment by serving as anchor points and ensuring proper teeth and jaw alignment. Different braces can be used on molars; their placement is essential for effective treatment. While there are challenges in caring for braces on molars, the benefits far outweigh them. Proper care and regular dental visits are crucial for oral health during orthodontic treatment. Understanding the role of molars in orthodontics helps patients appreciate the comprehensive nature of their treatment plan. Braces FAQs: Straightening Your Smile with Confidence Do molars need to be removed for braces? Not always. Removing molars (back teeth) for braces is a decision your orthodontist makes on a case-by-case basis. Some molars might need removal if there’s not enough room for proper alignment. However, orthodontists prefer to avoid extractions whenever possible. To create space, they’ll explore alternative techniques like palate expanders or dental arch expansion. Why can’t braces go on the back of teeth? Braces are typically placed on the front of teeth because they allow for better control and application
Inflamed Gums After Flossing: Causes, Prevention, and Treatment

Maintaining oral hygiene is essential for healthy teeth and gums. Flossing is a crucial part of this routine, yet many people experience inflamed gums after flossing. This article explores the reasons behind inflamed gums, how to prevent them, and effective treatment methods. Understanding Inflamed Gums After Flossing Flossing is designed to remove plaque and food particles from between teeth, where a toothbrush cannot reach. However, if you experience inflammation after flossing, it can be concerning. Inflamed gums are characterized by redness, swelling, and sometimes bleeding. This reaction can be due to various factors. Common Causes of Inflamed Gums After Flossing Several factors can cause inflamed gums after flossing. Understanding these can help prevent and manage the condition effectively. Incorrect Flossing Technique One of the primary reasons for inflamed gums is incorrect flossing technique. Using too much force or snapping the floss between teeth can injure the gum tissue, leading to inflammation. Gums are sensitive and need gentle care, even when flossing. Gingivitis Gingivitis is the inflammation of the gums due to plaque buildup along the gumline. If you have not been flossing regularly, the sudden introduction of flossing can irritate as it removes plaque and bacteria, leading to temporary inflammation. Tartar Buildup If plaque is not removed regularly, it hardens into tartar, irritating and inflaming the gums. Flossing can disturb this tartar, causing the gums to become inflamed. Allergic Reactions In some cases, an allergic reaction to the floss material can cause gum inflammation. This is less common but still a possible cause. Underlying Dental Conditions Certain dental conditions, such as periodontitis or abscesses, can cause inflammation. Flossing can exacerbate these issues, leading to inflamed gums. Prevention Strategies for Inflamed Gums After Flossing Preventing inflamed gums after flossing involves adopting proper techniques and maintaining overall oral hygiene. Here are some effective strategies: Use the Correct Flossing Technique Ensure you are flossing correctly. Use a gentle sawing motion to guide the floss between your teeth. Curve the floss into a C-shape around each tooth and gently slide it under the gumline. Avoid snapping the floss, as this can damage your gums. Floss Regularly Consistency is key in maintaining healthy gums—Floss at least once daily to remove plaque and food particles before they harden into tartar. Regular flossing helps prevent gum inflammation. Inflamed Gums After Flossing: Choose the Right Floss Select a floss that suits your needs. If you have sensitive gums, consider using a softer floss or a waxed version to reduce irritation. There are also flosses designed for people with braces or dental work. Rinse Your Mouth After flossing, rinse your mouth with water or an antibacterial mouthwash. This helps remove any dislodged particles and reduces the risk of inflammation. Brush Properly Brushing your teeth twice daily with a soft-bristled toothbrush helps maintain oral hygiene. Use fluoride toothpaste to strengthen your teeth and gums. Ensure you brush gently along the gumline to remove plaque without causing damage. Stay Hydrated Drinking plenty of water helps keep your mouth clean and your gums healthy. Water flushes out food particles and bacteria that can cause inflammation. Treatment for Inflamed Gums After Flossing If you experience inflamed gums despite preventive measures, there are several treatments you can consider. These treatments help alleviate symptoms and promote healing. Saltwater Rinse A simple saltwater rinse can reduce inflammation and promote healing. Mix half a teaspoon of salt in warm water and rinse your mouth for 30 seconds. Repeat this twice a day until the inflammation subsides. Cold Compress Applying a cold compress to the outside of your cheek can reduce swelling and numb the pain. Use a cold pack or a bag of frozen peas wrapped in a cloth. Apply it for 15-20 minutes several times a day. Over-the-Counter Anti-Inflammatories Non-prescription anti-inflammatory medications, such as ibuprofen, can help reduce pain and inflammation. Follow the dosage instructions and consult your dentist if you have any concerns. Topical Treatments Over-the-counter gels and creams designed for oral use can help soothe inflamed gums. Look for products containing benzocaine or hydrogen peroxide. Apply as directed on the package. Professional Dental Cleaning If tartar buildup is causing your gum inflammation, professional dental cleaning is necessary. Your dentist or dental hygienist will remove the tartar and plaque, reducing inflammation and preventing future buildup. Consult Your Dentist If your symptoms persist despite home treatments, consult your dentist. Persistent inflammation can be a sign of an underlying dental condition that requires professional attention. Your dentist can diagnose the issue and recommend appropriate treatment. Importance of Regular Dental Checkups Regular dental checkups are essential for maintaining oral health and preventing gum inflammation. During these visits, your dentist can identify and treat any potential issues before they become serious problems. Early Detection of Gum Disease Regular checkups allow your dentist to detect early signs of gum disease, such as gingivitis before it progresses to more severe conditions like periodontitis. Early treatment can prevent complications and keep your gums healthy. Professional Cleanings Professional cleanings remove plaque and tartar that regular brushing and flossing cannot. These cleanings help prevent gum inflammation and maintain overall oral health. Personalized Oral Care Advice Your dentist can provide personalized advice on oral care, including proper flossing techniques and the best products for your needs. This guidance can help prevent inflamed gums and other dental issues. When to Seek Immediate Dental Care if Inflamed Gums After Flossing While mild gum inflammation after flossing can be managed at home, certain symptoms require immediate dental attention. These include: Severe pain Persistent bleeding Swelling that does not subside Pus discharge from the gums Fever These symptoms can indicate a serious infection or other dental issues that need prompt professional treatment. The Role of Diet in Gum Health A balanced diet plays a crucial role in maintaining healthy gums. Certain nutrients are essential for gum health; incorporating them into your diet can help prevent inflammation. Vitamin C Vitamin C is essential for healthy gums. It helps in collagen production, which is crucial for gum tissue.
Bright Orange Plaque on Teeth: Causes, Prevention, and Treatment

Plaque on teeth is a common dental issue, but it can be particularly concerning when it turns bright orange. This article explores the causes of bright orange plaque, how to prevent it, and effective treatments to maintain a healthy, glowing smile. What is Plaque? Plaque is a sticky, colorless film of bacteria that forms on teeth. It develops when bacteria in the mouth mix with sugary or starchy foods. Plaque can lead to tooth decay, gum disease, and other dental problems if not removed regularly through proper oral hygiene practices. Understanding Bright Orange Plaque Bright orange plaque on teeth is less common than white or yellowish plaque. The distinct color can be alarming and often indicates a more specific cause. Unlike usual plaque, bright orange can be more noticeable and sometimes embarrassing. Causes of Bright Orange Plaque on Teeth Chromogenic Bacteria One of the primary causes of bright orange plaque is chromogenic bacteria. These bacteria produce pigments that can stain plaque orange. They thrive in environments where hygiene practices are inadequate. Chromogenic bacteria are often found in children and adolescents but can affect adults, too. Diet Diet plays a significant role in the formation of bright orange plaque. Foods and drinks with artificial coloring, such as candies, sodas, and certain processed foods, can contribute to the discoloration. Consuming these regularly can stain the plaque and give it a bright orange hue. Poor Oral Hygiene Neglecting oral hygiene is a major factor in developing bright orange plaque. Without proper brushing and flossing, plaque builds up and becomes discolored by food particles and bacteria. Skipping regular dental cleanings also allows plaque to accumulate and change color. Smoking Smoking or using tobacco products can cause plaque to turn bright orange. The tar and nicotine in tobacco products stain teeth and plaque, leading to a distinctive discoloration. Smokers are at a higher risk of developing this type of plaque due to the substances in tobacco. Symptoms and Risks of Bright Orange Plaque on Teeth The most obvious symptom of bright orange plaque is the visible discoloration of teeth. The orange tint can be unsightly and affect one’s confidence. This type of plaque is usually noticeable near the gum line and between teeth. Bad Breath Bright orange plaque can contribute to bad breath. The bacteria that cause the discoloration also produce sulfur compounds, leading to an unpleasant odor. Maintaining good oral hygiene is crucial to prevent bad breath caused by plaque buildup. Tooth Decay and Gum Disease Bright orange plaque can lead to more serious dental issues if left untreated. The bacteria in plaque produce acids that erode tooth enamel, causing cavities. Additionally, plaque buildup can inflame the gums, leading to gingivitis and periodontal disease. Preventing Bright Orange Plaque on Teeth Maintain Good Oral Hygiene Maintaining good oral hygiene is the best way to prevent bright orange plaque. Brush your teeth at least twice a day with fluoride toothpaste. Make sure to brush for two minutes, covering all surfaces of your teeth. Floss daily to remove plaque between teeth that your toothbrush can’t reach. Regular Dental Checkups Visit your dentist regularly for checkups and cleanings. Professional cleanings remove plaque and tartar that you might miss at home. Your dentist can also provide personalized advice on maintaining oral hygiene and preventing plaque buildup. Diet and Nutrition Watch what you eat and drink to prevent bright orange plaque. Limit foods and beverages with artificial coloring and high sugar content. Eat a balanced diet rich in fruits, vegetables, and whole grains. Drinking water after meals can also help rinse away food particles and bacteria. Quit Smoking If you smoke or use tobacco products, consider quitting. Smoking not only stains teeth and plaque but also increases the risk of gum disease and oral cancer. There are many resources available to help you quit smoking and improve your oral health. More than 80% of American adults suffer from periodontal disease caused by plaque formation. Treating Bright Orange Plaque on Teeth Professional Dental Cleaning The most effective treatment for the bright orange plaque is professional dental cleaning. During a cleaning, your dentist or hygienist will remove plaque and tartar from your teeth. They will also polish your teeth to remove surface stains and make them look brighter. Scaling and Root Planing Your dentist may recommend scaling and root planing for more severe cases of plaque buildup. This deep cleaning removes plaque and tartar above and below the gum line. It also smooths the root surfaces to help prevent future plaque buildup. Whitening Treatments If bright orange plaque has stained your teeth, whitening treatments can help. Your dentist can provide professional whitening treatments to lighten the stains and improve the appearance of your teeth. Over-the-counter whitening products are also available, but professional treatments are more effective. Antibacterial Mouthwash for Bright Orange Plaque on Teeth Using an antibacterial mouthwash can help reduce the bacteria that cause plaque. Look for mouthwashes with fluoride to help strengthen your teeth. Rinsing with mouthwash after brushing and flossing can help keep your mouth clean and reduce plaque buildup. Home Remedies to Remove Bright Orange Plaque on Teeth Baking Soda Baking soda is a natural abrasive that can help remove plaque. Mix a small amount with water to create a paste, and brush your teeth with it once a week. Baking soda can help scrub away plaque and surface stains but don’t use it too often, as it can be abrasive to your enamel. Hydrogen Peroxide Hydrogen peroxide has antibacterial properties that can help reduce plaque. Dilute it with equal parts water and use it as a mouth rinse. Swish it around your mouth for 30 seconds, then spit it out. Be careful not to swallow hydrogen peroxide, as it can be harmful. Oil Pulling Oil pulling is an ancient practice that involves swishing oil in your mouth to remove bacteria. Coconut oil is a popular choice due to its antibacterial properties. Swish a tablespoon of coconut oil in your mouth for 15-20 minutes, then spit it out.
Understanding the Connection Between Gum Pain and Headaches

Gum pain and headaches are seemingly unrelated issues that can often be connected surprisingly. While many people might not immediately associate dental problems like gum pain with headaches, a significant correlation exists between the two. In this article, we discuss the various causes, symptoms, and potential treatments for gum pain that can lead to headaches, offering insights to help you understand and manage these interconnected health concerns. The CDC found that severe gum disease, or periodontitis, affects about 9 percent of adults in the US. About 5.08 percent of adults between 20 and 64 years old have some form of moderate or severe periodontal disease, and 8.52 percent have any gum disease. This can lead to tooth decay, which one in four adults in the US has. How Gum Pain Can Lead to Headaches Gum pain refers to discomfort, soreness, or irritation in the gums, which can arise from various dental issues. When left untreated, these issues can escalate and potentially lead to headache. One of the primary mechanisms linking gum pain to headaches is referred pain. Referred pain occurs when pain signals from one part of the body are perceived as originating from another location. In this case, dental issues such as gum inflammation or infection can radiate pain to the head and neck area, triggering headaches. Moreover, persistent gum pain can lead to stress and tension in the facial muscles and jaw. This muscular tension, known as bruxism (teeth grinding) or clenching, is a common response to dental discomfort. Over time, chronic clenching and grinding can strain the head and neck muscles, resulting in tension headache or migraines. Common Causes of Gum Pain Several dental conditions can cause gum pain, each potentially contributing to headaches: Gingivitis and Periodontitis: Gum pain often arises from gum diseases such as gingivitis (inflammation of the gums) and periodontitis (advanced gum disease). These conditions are typically caused by bacterial infection, leading to swelling, redness, and tenderness of the gums. If left untreated, gingivitis can progress to periodontitis, where the gums pull away from the teeth, forming pockets that accumulate more bacteria and pus. The resulting inflammation and infection can cause significant gum pain and contribute to headaches. Dental Abscess Is also the Reason for Gum Pain and Headaches: An abscessed tooth or gum abscess occurs when a bacterial infection causes a pocket of pus to form in the tooth or gums. This infection can lead to severe gum pain, swelling, and throbbing headache due to the pressure created by the pus-filled abscess. Bruxism: As mentioned earlier, bruxism is the habitual grinding or clenching of teeth, often in response to stress or dental discomfort. The continuous strain on the jaw muscles and temporomandibular joint (TMJ) can lead to jaw pain, facial soreness, and tension headaches that radiate to the temples and forehead. Tooth Sensitivity: Gum recession or enamel erosion can expose the sensitive roots of teeth, leading to sharp pain when exposed to hot, cold, sweet, or acidic foods and beverages. This dental sensitivity can cause discomfort that extends to headaches, especially if the pain is chronic or severe. Symptoms of Gum Pain and Associated Headaches Recognizing the symptoms of gum pain and headaches is crucial for timely intervention and treatment. Here are the common symptoms to watch out for: Gum Pain Persistent soreness, tenderness, or swelling of the gums can indicate various dental issues such as gum disease, infections, or trauma. Tooth Pain Sharp or throbbing pain in the teeth, especially when chewing or biting down, suggests possible tooth decay, abscess, or sensitivity. Headaches Dull or throbbing headaches that worsen over time, often accompanied by facial tenderness or jaw pain, may be linked to dental problems like bruxism or gum inflammation. Jaw Pain Discomfort or clicking sounds when opening and closing the mouth may indicate temporomandibular joint (TMJ) disorders or teeth grinding (bruxism). Bad Breath Persistent bad breath despite regular oral hygiene practices can indicate underlying gum disease or infection. Swollen Gums Red, swollen gums that bleed easily, particularly during brushing or flossing, are typical symptoms of gingivitis or periodontitis. If you experience any of these symptoms, it is essential to consult with a dental professional for a comprehensive evaluation and appropriate treatment. Treating Gum Pain to Alleviate Headaches Effective treatment of gum pain not only improves oral health but also helps alleviate associated headache. Treatment options may include: Professional Dental Cleaning Scaling and root planing remove plaque and tartar buildup from the teeth and gums, which helps reduce inflammation and prevent gum disease progression. Antibiotics Prescription antibiotics to treat bacterial infections causing gum disease or abscesses, aiming to eliminate the infection and alleviate associated pain. Root Canal Therapy Treatment for infected tooth roots (root canal treatment) to alleviate pain and prevent further complications such as abscesses. Pain Relief Over-the-counter pain medications (e.g., ibuprofen, acetaminophen) to manage discomfort and headaches associated with dental issues. Custom Mouthguards A dentist customizes night guards or splints to prevent teeth grinding (bruxism) and alleviate jaw muscle tension, which can contribute to headaches. Surgical Intervention In severe cases of gum disease or abscesses, surgical procedures such as gum surgery or tooth extraction may be necessary to restore oral health and prevent complications. Preventive Measures for Gum Pain and Headaches Preventing gum pain and associated headaches starts with adopting good oral hygiene practices and regular dental check-ups: Brushing and Flossing Brush your teeth at least twice daily with fluoride toothpaste and floss daily to remove plaque and prevent gum disease. Routine Dental Visits Prevent Gum Pain and Headaches Schedule regular dental cleanings and exams (every 6 months or as your dentist recommends) to detect and treat dental issues early. Healthy Diet Eat a balanced diet of fruits, vegetables, and calcium to support oral health and strengthen teeth and gums. Avoid Tobacco Quit smoking and avoid tobacco products, as they contribute to gum disease and oral infections and hinder healing after dental treatments. Stress Management Practice stress-reducing techniques such as meditation, yoga, or exercise to minimize teeth grinding (bruxism)
How to Prepare a Tooth for a Crown

Getting a dental crown is a common procedure in modern dentistry. Crowns restore a tooth’s shape, strength, and function after damage. Whether the damage is due to decay, a large filling, or a fracture, a crown can help protect and strengthen the tooth. This article will walk you through the detailed steps of how to prepare a tooth for a crown, ensuring you understand the entire process. Understanding Dental Crowns Dental crowns are caps placed over a tooth to restore shape, size, and appearance. They can be made from various materials, including metal, porcelain, resin, or ceramic. Crowns are used for multiple reasons, such as to protect a weak tooth, restore a broken tooth, cover a dental implant, or improve the appearance of a discolored or misshapen tooth. Types of Dental Crowns There are different types of dental crowns, each with its benefits. Metal crowns, made from gold, platinum, or base-metal alloys, are known for their durability and strength. Porcelain-fused-to-metal crowns provide a more natural tooth color and are suitable for front and back teeth. All ceramic or all-porcelain crowns offer the best natural color match and are ideal for people with metal allergies. Resin crowns are less expensive but wear down over time and are more prone to fractures. Initial Consultation for Prepare a Tooth for a Crown The first step in preparing a tooth for a crown is an initial consultation with your dentist. During this visit, your dentist will examine the tooth and determine if a crown is the best option for treatment. They will take X-rays to assess the roots of the tooth and the surrounding bone. If the tooth has extensive decay or there is a risk of infection, a root canal treatment may be necessary before the crown is placed. Treatment Plan: Prepare a Tooth for a Crown Your dentist will develop a treatment plan based on the examination and X-rays. This plan will outline the steps to prepare your tooth for a crown. It will also include details about the type of crown used and the procedure’s timeline. Your dentist will discuss the treatment plan with you and address any questions or concerns you may have. Prepare a Tooth for a Crown Once the treatment plan is in place, the next step is to prepare the tooth for the crown. This involves several key steps to ensure the tooth is properly shaped and ready for the crown to be placed. Anesthesia to Prepare a Tooth for a Crown The first step in the preparation process is administering local anesthesia to numb the tooth and surrounding area. This ensures you do not feel any pain during the procedure. Your dentist will use a needle to inject the anesthesia into the gums near the tooth that will receive the crown. Removing Decay and Old Fillings After the anesthesia takes effect, your dentist will remove any decay from the tooth. If the tooth has an old filling, it will also be removed. This step is crucial to ensure the tooth is free of decay or infection before placing the crown. Reshaping the Tooth When Prepare a Tooth for a Crown Next, the dentist will reshape the tooth to make room for the crown. They will trim the tooth on the top and sides using a dental drill. The amount of teeth removed depends on the type of crown being used. For example, metal crowns require less tooth removal than porcelain or ceramic crowns. The goal is to create a tooth shape that allows the crown to fit snugly and securely. Building Up the Tooth Sometimes, the tooth must be built up before the crown can be placed. This is often necessary if a large portion of the tooth is missing due to decay or damage. Your dentist will use a filling material to build up the tooth’s core, providing a solid foundation for the crown. Taking Impressions to Prepare a Tooth for a Crown After the tooth is properly shaped, impressions are taken. These impressions create a custom crown that fits perfectly over the prepared tooth. Digital Impressions Many modern dental offices use digital impression technology to create a 3D image of the tooth. This process involves using a small wand to scan the tooth and surrounding area. The digital images are then sent to a dental lab, where the crown is designed and manufactured. Digital impressions are more accurate and comfortable than traditional impressions. Traditional Impressions In some cases, traditional impressions may be used. This involves placing a putty-like material in a tray and pressing it against the tooth. The material sets and creates a mold of the tooth. The mold is then sent to a dental lab, where the crown is made. While traditional impressions are effective, they can be uncomfortable for some patients. The global dental crowns and bridges market size was valued at USD 2.85 billion in 2018 and is projected to reach USD 4.56 billion by 2026. Source. Temporary Crown Placement While waiting for the permanent crown, your dentist will place a temporary crown over the prepared tooth. This temporary crown protects the tooth and maintains its function until the permanent crown is ready. Creating the Temporary Crown The temporary crown is usually made from acrylic or composite resin. Your dentist will shape the material to fit over the prepared tooth. It is then cemented in place with temporary dental cement. The temporary crown is not as strong as the permanent crown, so avoiding chewing hard or sticky foods that could dislodge it is important. Caring for the Temporary Crown While you have a temporary crown, it is important to take care of it to avoid any issues. Avoid chewing on the side of the mouth with the temporary crown, and practice good oral hygiene by brushing and flossing gently around the crown. If the temporary crown becomes loose or falls off, contact your dentist immediately to have it re-cemented. Permanent Crown Placement Once the permanent crown is ready, you will return


